Author: Gorazd Hladnik, Health Lord (Gospodar Zdravja)
Social and technological development are becoming faster and demanding adjustments of social subsystems, including healthcare. Ahead of us lie new and ever bigger challenges. While in the past, people emphasized social equality, human rights, and in recent years, environmental protection issues, modern development increasingly brings to the forefront the problem of information pollution, manipulation of information, and fake news. The generators of these issues are primarily groups and individuals who hold political and/or economic power with distinctly expressed partial interests that they assert. It is obvious that this last problem mentioned is the biggest and most complex, as it has the potential to shape public opinion and even cultural behavioural patterns, thus influencing the perception of other social issues. This is most evident in critical situations in society, such as ecological threats, pandemics and their management, as well as wars in Ukraine and Palestine. In all of these cases, there have been and continue to be manipulations and fake news, often too much unnecessary information. A particular problem is the uncontrolled penetration of artificial intelligence and the control over individuals enabled by modern technologies and analytical algorithms, primarily by leading application providers.
Individuals’ main challenges are more personally oriented, and yet, besides concerns for health, social status, material well-being, and competencies, an area that is very important and concerning for each of us is the realm of information and data collected about us by various actors, thus the issue of privacy and security.
Information pollution and manipulation are not only the challenges faced by global society, but also affect healthcare. It’s not just about various forms of economic propaganda, but about the overall pressure from printed, electronic media, and the internet on health topics, as well as the dissemination of unverified, sometimes even extreme views of certain social groups and media outlets. The voices of healthcare professionals and public health are lost in the flood of one-sided or misleading information.
*Better resolution visuals are available in PPT presentation at the end of this article
In the field of health management, there has traditionally been an asymmetry of knowledge and access to information. Despite patients’ declared ownership of health data, the actual role of controllers is played by governmental institutions, healthcare providers, and health insurance companies. Patients remain with limited accessibility and transparency of their health data dispersed among various actors.
It is true that in recent times, the gaps between professionals and patients in knowledge and access to health and treatment information have narrowed. However, greater health literacy among patients does not change the fact that the patient does not manage their personal health data. Therefore, the situation is still far from ideal. This is the fundamental reason for the poorer engagement of patients in prevention and treatment, which is one of the biggest challenges in healthcare.
*Better resolution visuals are available in PPT presentation at the end of this article
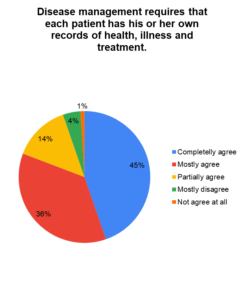
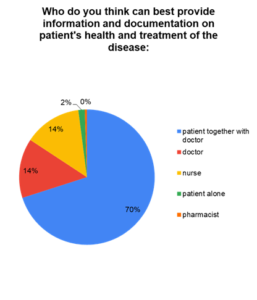
It is high time for patients to become the actual owners and managers of health information, data, and documents. By doing so, patients take on responsibility for their health and gain additional motivation for better health and disease management. Our own research outcomes confirm that patients understand and want to take over ownership and management of their health data alongside their personal physicians.
*Better resolution visuals are available in PPT presentation at the end of this article
Health-related data should be consolidated in a single, unified platform accessible and manageable by patients, ensuring completeness, comprehensiveness, accuracy, and reliability. This comprehensive repository should encompass healthcare documents, personal health history, familial traits, genetic information, and relevant bio-parameters. Upholding privacy, safety, accessibility, ease of management, user control, portability, transferability, interoperability, and exchangeability with patients’ consent are paramount considerations. While anonymized data may serve scientific and research purposes, individuals should derive tangible benefits from sharing personal data with biobanks.
The ownership and active management of health data by patients hold pivotal significance for multiple reasons, reflecting the evolving healthcare landscape and the burgeoning emphasis on patient-centric care. Such ownership facilitates patient empowerment and informed decision-making, fosters improved communication with healthcare providers, streamlines care coordination, enables enhanced health monitoring, and paves the way for personalized and precision medicine.
As healthcare systems undergo continuous transformation, patient ownership and management of health data are poised to remain focal points in advancing patient-centered and efficient care. This is the case despite several challenges related to patient health data management persisting, including security concerns, interoperability, control, data accuracy and quality as well as ethical use. Balancing the interests of individuals, healthcare providers, researchers, and technology companies is a complex challenge where patients and health providers should have top priority.
Technological Infrastructure, patient engagement and legal and regulatory compliance are further important factors influencing the dynamics of patient empowerment in health data management.
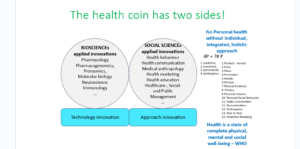
The progress and adaptation of the healthcare sector to the new societal environment are notably sluggish, arguably the slowest among all sectors. This is particularly evident in the areas of informatization, communication, psycho-social approaches, and collaboration among stakeholders. The predominant focus on biotech innovations underscores the fact that medicinal progress is primarily driven by technological advancements. Unfortunately, the organizational, communicational, and interpersonal aspects of healthcare processes often take a backseat, as illustrated below:
*Better resolution visuals are available in PPT presentation at the end of this article
Only appropriate combination of bio-tech and social innovation in healthcare leads to sustainable progress.
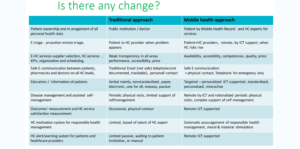
The sustainable progress in healthcare necessitates a balanced integration of biotech and social innovation. Consequently, our focus is on introducing a novel healthcare approach, called as “mobile health management,” alongside the implementation of appropriate ICT tools.
The historical evolution of ICT and Electronic Health Records (EHR) in healthcare has predominantly aimed at supporting transactions, financial control, identity verification, and professional credentials. While later stages introduced IT support for documents and processes within healthcare, including EHR, e-prescriptions, and seamless care, there remains a notable absence of ICT support for patients and interoperability with healthcare providers. Recent advancements, such as the Mobile Health Record by Gospodar zdravja – Healthlord, facilitate collaboration between patients and healthcare providers, revolutionizing health and disease management. These tools enable new approaches such as Personal Health Records (PHR) with diaries, health monitoring, active triage, secure electronic communication, e-education systems, and active remote disease management. They also offer telemedicine and tele-pharmacy services, alongside motivation and alert systems to enhance adherence. Without such ICT support, innovative approaches like mobile health management would not be feasible.
Mobile Health Management is an interdisciplinary, patient-centered approach to health management supported by advanced information and communication technologies. Its primary aim is to achieve the health targets of individual patients, essentially constituting health marketing supported by modern communication tools.
Health marketing solely targets efficiently supporting patients to manage their health, devoid of any sales or profit motives. However, it involves recognizing individual needs, targeting specific patients, patients’ segmentation, adapting interaction approaches, and personalizing communication. It addresses several key challenges faced by the global healthcare sector, including low patient empowerment and adherence levels (at only 50% in EU, estimated associated EU annual costs are EUR 125 bn), healthcare capacity shortages, funding deficits, administrative burdens, underutilized competencies of pharmacists, and issues of trust and reputation.
Mobile health management empowers patients not only with knowledge but also with ownership and management of all personal health data, facilitated by dedicated ICT tools like the Mobile Health Record. It introduces new services, approaches, and interactions among healthcare experts and patients, including HC services/suppliers’ selection based on performance, accessibility, and affordability, proactive remote triage, remote organization and scheduling of HC services, safe electronic communication between patients, pharmacists, and doctors on all HC levels, targeted and personalized patient education/information, remote disease management, assisted self-management, and outcomes measurement, and HC service satisfaction measurement. It could be supported by a motivation system for responsible health management and an alert/warning system for patients and healthcare providers. Mobile health management accelerates the teamwork of all HC experts – physicians, specialists, secondary institutions, and other healthcare providers, including community pharmacists in primary and secondary care. It could indirectly increase HC capacities by involving remote collaboration with tele-medicine and tele-pharmacy and have a positive impact on health-economic outcomes as well.
Mobile health management includes social innovations like new patient motivation approaches, new services, and provider approaches. Social innovations include innovative approaches in social group interactions, new ways of interaction between healthcare providers and patients, interactions within the HC public system-patients, interactions among patients, as well as interactions between healthy individuals (caregivers) and patients. Roles of involved healthcare providers and patients are changing, starting with ownership and management of health data. Patients’ level of involvement in decision-making and management of health is significantly increased, leading to increased responsibility. Mobile health management represents new approaches in communication, new communication channels, adapted intensity, frequency, and style of communication, as well as new content, amount, and design of messages. A crucial element is differentiation, segmentation, and targeting of patients to achieve personalization of communication and services, improved social interaction, and encouragement. The entire healthcare marketing mix should be thoroughly followed. A key element of mobile health management is the motivation system, including psychological, moral, and material elements.
The disparities between traditional and mobile health management approach are striking.
*Better resolution visuals are available in PPT presentation at the end of this article
ICT solutions like Healthlord are indispensable. They support all stakeholders and support introduction of mobile health approach. The key functionalities and interconnections are demonstrated bellow

*Better resolution visuals are available in PPT presentation at the end of this article
The evidence supporting the effectiveness of mobile health management (mHealth) compared to conventional methods is robust and involve enhanced chronic disease management, improved medication adherence, expanded access to healthcare, positive influence on health behaviour, remote monitoring and early disease detection as well as improved cost-effectiveness and enhanced service quality.
However, the implementation process is time-consuming due to various entry barriers. One primary obstacle lies in the divergent interests of patients and healthcare professionals, as identified in our research. Health professionals have deemed the following functionalities of ICT tools significantly less important compared to patients’ perceptions:
- Remote access to healthcare services and products from home.
- Provision of pricing information for healthcare services and treatment products.
- Transparency and insight into the accessibility and performance of healthcare providers.
- Access to remote second opinions on health and illness.
- Utilization of E-safe consultations.
In addition to these challenges, there are several other entry barriers, both formal and informal, related to patients, healthcare providers, the regulatory environment, procurement processes, and various other factors.
In conclusion, patients are encouraged to play an active role in managing their health, which includes taking charge of their health data. Collaborating with healthcare providers, patients can explore the opportunities for improving their health through mobile health management.
Download the article with all visuals by clicking here: Patient health data ownership and mHealth managemen ang_HealthLord


